In today’s health care environment, the stakes for accurate and compliant documentation have never been higher, especially with dementia coding. Under the CMS-HCC V28 model, dementia maps to a single risk-adjusted value regardless of severity. But that simplicity masks a deeper risk: vague or incomplete documentation can lead to costly consequences.
In the era of Risk Adjustment Data Validation (RADV) audits and heightened payer scrutiny, it’s not just the diagnosis that matters, it’s the documentation that tells the full story. Without clear, specific clinical support, even a valid dementia diagnosis can result in financial penalties, clawbacks, and reputational damage.
The danger of "technically correct" coding
It’s a familiar scenario: A provider documents “memory issues” or “history of dementia” and selects an HCC code (125, 126, or 127).
The code is technically accurate—and the diagnosis is real.
But to an auditor, this chart tells an incomplete story. And incomplete stories raise red flags.
In 2023, CMS projected over $4.7 billion in RADV recoveries across a 10-year period, with increased scrutiny of diagnoses that are often miscoded or insufficiently supported. RADV auditors and payer Special Investigation Units (SIUs) are trained to evaluate the clinical context—not just the presence of a code
They ask:
- Is there sufficient evidence to support an active diagnosis?
- Is the condition being monitored, assessed, or addressed during the visit?
- Are symptoms and severity documented and aligned with the diagnosis?
If the answer is unclear, the diagnosis—and its associated risk adjustment—may be invalidated.
Why dementia documentation is under the microscope
Dementia is particularly vulnerable to audits. Despite different ICD-10-CM codes, all dementia diagnoses map to a single risk score under HCC V28, which can incentivize vague documentation. Yet dementia is a progressive condition, not
According to the Alzheimer’s Association, 6.7 million Americans aged 65+ are living with Alzheimer’s dementia—a number projected to nearly double by 2050. Under-documentation not only creates compliance risk but underrepresents patient needs. Comorbidities like depression and delirium further complicate diagnosis and increase the need for clinical clarity. a static one. Records should reflect ongoing changes in cognition, behavior, and function.
In short, dementia documentation that lacks specificity is low-hanging fruit for auditors.
Key elements of defensible dementia documentation
To protect against audit risks, documentation must move beyond simply listing "dementia" in the problem list or assessment. Strong, defensible documentation includes:
1. Active status
Dementia must be documented as an active condition—not just history. Providers should demonstrate monitoring or management.
Example:
- “Cognitive decline worsening; discussed need for increased supervision.”
- "Stable; continuing current dementia meds.”
- “Managing symptoms of confusion and nighttime wandering.
Use the MEAT framework—Monitor, Evaluate, Assess/Address, Treat—to support audit readiness.
2. Severity and impact
Use ICD-10-CM codes (F01–F03, G30 categories) to:
- Specify etiology (e.g., Alzheimer's, vascular dementia)
- Indicate severity: mild, moderate, or severe
- Note behavioral disturbances (e.g., aggression, wandering)
- Describe functional impact (e.g., difficulty managing medications)
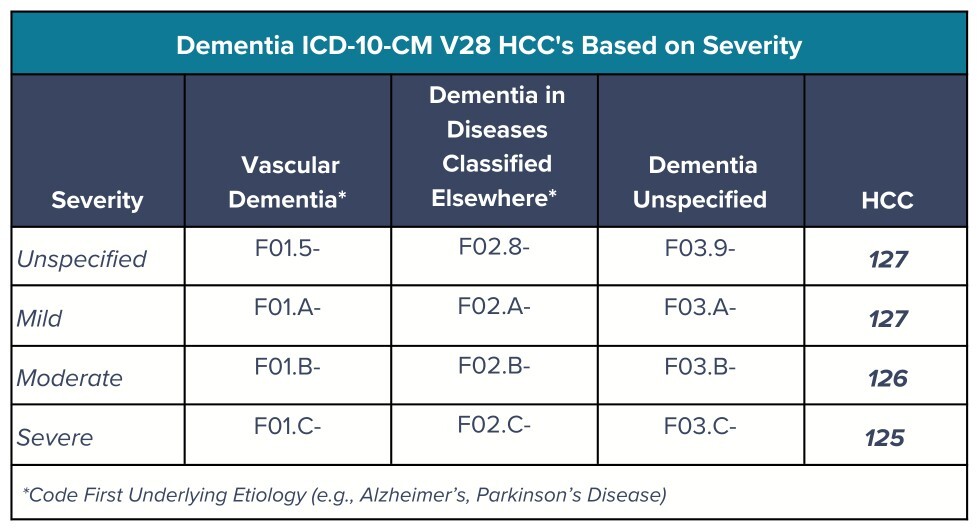
ICD-10-CM codes and HCCs for dementia include:
Example: “Patient exhibits moderate dementia with increased disinhibition and requires reminders to bathe and take medications.”
Code F02.B18 (unspecified dementia, moderate, with behavioral disturbance) maps to HCC 126, capturing added symptom burden.
Tip: Link symptoms and functional limitations directly to the diagnosis.
3. Monitoring or management plan
Show how the condition is addressed through testing, care planning, referrals, or medication.
Example: “Referred to neurology for evaluation. Developed a care plan and educated caregiver on fall prevention.”
4. Associated symptoms
Document behavioral, neurological, or psychiatric symptoms such as agitation, hallucinations, or wandering.
Many ICD-10-CM codes reflect behavioral disturbances. Definitions and documentation standards are also outlined in the DSM-5-TR and American Psychological Association guidelines.
Protecting revenue starts with telling the full story
Dementia is a complex, progressive condition—and documenting it requires more than checking a box. To stay ahead of audits and justify risk-adjusted payments, health systems must treat documentation as a strategic asset.
Building an audit-ready culture starts with provider education on specificity, supported by EHR templates that prompt for detail without burden. Embedding coding professionals into workflows and conducting targeted reviews for high-risk conditions like dementia can reduce denials and retroactive losses.
Digital cognitive assessment tools like those offered by Creyos further strengthen this strategy. These tools support diagnostic accuracy and generate defensible documentation. This includes providing objective evidence of cognitive function aligned with HCC criteria, enabling active monitoring, and facilitating the development of care plans.
In value-based care, documentation isn’t just a billing requirement, it’s a clinical narrative. When that story is complete, specific, and backed by objective cognitive data, it safeguards compliance, reinforces care quality, and protects the revenue your patients and providers depend on.
When compliance and care quality go hand-in-hand, digital tools and disciplined documentation aren’t just helpful— they’re your best defense.
About the author
Emily Montemayor is a distinguished health care professional with over a decade of specialized expertise in revenue integrity, compliance, CDI, provider education, and auditing. As the medical coding support manager at Creyos and a recognized subject matter expert, she has been instrumental in driving optimized reimbursement strategies and reinforcing revenue integrity for our clients. Her influence extends globally, where she has trained health care professionals and pioneered innovative coding solutions. Her thought leadership is showcased through published articles in AAPC magazines and impactful collaborations with MedLearn Media on book editorials and educational webcasts. Montemayor is dedicated to advancing the health care industry through her commitment to education, compliance excellence, and innovative content development.
