With the CMS-HCC V28 model emphasizing dementia in risk adjustment and its rising prevalence, dementia is emerging as a top priority for health systems.
Yet, the challenge is clear: many still struggle to integrate effective screening into workflows that align with value-based care (VBC). The challenge isn’t just detection—it’s about finding a way to identify early-stage dementia that supports better patient outcomes while ensuring financial viability.
This article explores how early dementia screening can:
● Enhance risk adjustment accuracy: Capturing dementia diagnoses earlier aligns risk adjustment factor (RAF) scores with patient complexity, unlocking critical care resources.
● Reduce costly interventions: Early detection helps prevent emergency visits, hospitalizations, and late-stage care, lowering costs for full-risk-bearing organizations.
● Leverage scalable technology: Digital tools enable shorter, more accessible assessments, making early screening feasible in primary care.
Closing risk adjustment gaps
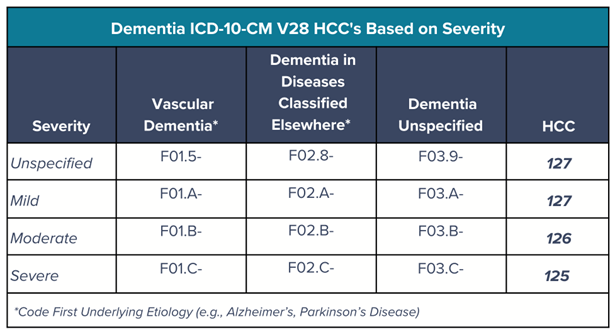
As the CMS-HCC V28 model enters its second year in 2025, health systems must adapt to updated coding for more accurate risk adjustment and VBC alignment. One of the most significant updates expands dementia classification, improving documentation and reimbursement through increased specificity in ICD-10-CM and expanded HCC categories.
Previously, coding early-stage dementia in ICD-9-CM often required multiple codes, which could lead to administrative inefficiencies and potential errors. V28 streamlines this with mild, moderate, and severe categories, assigning a RAF value of 0.341. This specificity enhances coding accuracy and supports earlier recognition, essential for proactive care.
Consider, too, that nearly 50 percent of dementia cases in the U.S. go undiagnosed, partly due to screening tools that detect only late-stage symptoms—limiting not only diagnostic accuracy but also medical necessity documentation and reimbursement. More sensitive tools can capture dementia earlier, aligning diagnosis rates with actual prevalence while securing financial support. With VBC’s shift, health systems can finally close this care gap—if they adopt the right detection tools.
Avoiding missed reimbursement: How to improve dementia coding
Here are some dementia coding essentials under VBC:
● Understand HCC categories for dementia severity:
○ HCC 127 – Unspecified/Mild Dementia
○ HCC 126 – Moderate Dementia
○ HCC 125 – Severe Dementia
● Capture underlying etiologies with causal language (e.g., Dementia due to Parkinson’s disease) to document both the etiology and dementia accurately.
● Assess additional underlying factors and comorbidities, such as: coronary artery disease, stroke history, and cerebrovascular disease.
● Missed risk adjustment opportunities occur when unspecified cognitive impairment codes (e.g., R41.8- or G31.84) replace more specific dementia diagnoses.
Reducing dementia impacts on population health
Without investment in preventive care and dementia screening, full-risk-bearing organizations will face growing financial strain. Early detection is critical—not just for patient outcomes but also for reducing system-wide costs.
By integrating routine cognitive screening, providers can identify dementia alongside comorbidities such as cardiovascular disease and diabetes, which research has shown can accelerate cognitive decline.
Addressing these conditions early lowers hospitalizations, emergency visits, and long-term care costs while empowering patients and families to make informed decisions. With dementia-related health care costs exceeding $300 billion annually, reactive approaches are unsustainable. Proactive screening reduces high-cost interventions, improves care coordination, and aligns with VBC models that emphasize prevention over crisis management.
Getting provider and patient buy-in on dementia screening
Despite advances in research and technology, adoption of dementia screening remains slow. Some of the most pressing challenges involve getting providers and patients to embrace change.
Providers today face compounding systemic challenges including significant worker shortages, administrative burden, workflow and time limitations, and the pressures to ensure financial sustainability. Common screeners like MMSE, SLUMS, and MoCA often miss early cognitive impairment, leading to delays in diagnosis and higher population health costs, especially in diverse and non-standard cases. These delays also contribute to higher population health burdens by allowing comorbid conditions like cardiovascular disease, diabetes, and depression to worsen cognitive decline.
Patients also face barriers—navigating insurance, accessing providers, and overcoming stigma, which more than 57 percent of physicians report as a deterrent to early screening. Routine assessment creates opportunities to educate patients, address stigma, and identify modifiable risk factors that help prevent dementia. Without it, undiagnosed dementia increases care needs and health care costs.
Digital cognitive tools: A scalable solution
Technology-driven screening tools can detect cognitive impairment early (before comorbidities worsen and outcomes decline) while reducing provider burden. Unlike paper tests, digital solutions integrate seamlessly into workflows, standardize scoring, and provide real-time insights for timely intervention. Digital tools also improve accessibility by offering multilingual options and accommodations for visual, audio, and learning needs.
In VBC, early cognitive impairment detection supports proactive comorbidity management, reducing hospitalizations and long-term costs. Scalable technologies, including electronic medical record (EMR) integration and automated reporting, enhance diagnostic confidence while preserving provider time.
Pilot programs show that digital screeners, administered in under three minutes, are effective across diverse health care settings, demonstrating ease of implementation and strong provider adoption. Successful rollouts often involve targeted provider training and physician champions to facilitate seamless integration.
Achieving a more sustainable future of dementia care
Utilizing sensitive screening tools and the enhanced specificity of the V28 model ensure precise documentation of dementia severity, improving risk stratification, optimizing reimbursement, and strengthening VBC alignment. By supporting early intervention and proactive care planning, digital cognitive assessments enhance dementia detection, promote population health, and drive financial sustainability in evolving health care models.
About the author
Emily Montemayor, CCS, CMBCS, COC, CPC, CPMA, is a distinguished health care professional with over a decade of specialized expertise in revenue integrity, compliance, CDI, provider education, and auditing. As the medical coding support manager at Creyos and a recognized subject matter expert, she has been instrumental in driving optimized reimbursement strategies and reinforcing revenue integrity for our clients. Montemayor‘s influence extends globally, where she has trained health care professionals and pioneered innovative coding solutions. Her thought leadership is showcased through published articles in AAPC magazines and impactful collaborations with MedLearn Media on book editorials and educational webcasts. She is dedicated to advancing the health care industry through her commitment to education, compliance excellence, and innovative content development.
