Data: The missing link in value-based care
The shift away from fee-for-service to value-based care has been underway for some time, and yet payers and providers still haven’t developed the right strategies to move the needle on cost and quality goals. Underlying each health care organization is a treasure trove of power: mountains and mountains of data with the potential to power risk adjustment and quality improvement programs. By making better use of their data, providers can pinpoint and prioritize critical care gaps with incredible accuracy, helping them make huge strides in improving outcomes and lowering costs.
Participation in (and pressure to participate in) value-based care models is growing at a rapid rate. As of January 1, the Medicare Shared Savings Program (MSSP), the largest accountable care program in the country, served 11.2 million beneficiaries alone. And from 2017-2022, up to 9 in 10 physician practices were participating in at least one value-based care model.
But the challenge of successfully meeting the goals of lowered costs and improved quality under value-based care persists. Most payers and providers need to make significant changes to their data infrastructure and workflows but have been forced to balance their technology needs while facing an array of challenges: clinical workforce shortages, economic pressures, and heightened compliance scrutiny.
The way forward? Better data management to power that technologies that drive outcomes. Each patient encounter generates a wealth of data, and yet too often that data is untapped, stuck in unstructured clinical notes, varying formats, and stored in data siloes. Health care organizations that want to succeed in value-based care need to bridge the gap between their operational reality and data ambition.
The state of technology in value-based care
Last month, Reveleer, in partnership with The Harris Poll and Mathematica, released a comprehensive survey report: “The State of Technology in Value-Based Care.” The report surveyed over 200 U.S.-based directors, executives, and C-suite leaders, focusing on approaches to data management, artificial intelligence, and cybersecurity and the connection to their value-based care goals.
One of the most notable findings was that health care leaders experience a gap in their ability to achieve value-based care goals: effective data management.
“Industry leaders widely acknowledge that data provide a competitive advantage, but siloed systems and quality challenges continue to block its full utility,” stated the report.
The challenges are significant: making use of complex, varied, siloed data to pinpoint and close care gaps. Resolving these challenges requires substantial technology transformation. Fortunately, innovative new technology including advances in artificial intelligence (AI) can bridge the gap.
Top 4 data issues challenging the future of value-based care
1. Data management
Nearly all leaders surveyed (97 percent of providers and 96 percent of payers) agree that strong data management gives them a competitive edge. Strong data management delivers a more complete picture of patient health, powers care gap closure, improves quality ratings, and helps retain and attract patients and members.
Nevertheless, system integration is a challenge. Currently, only a third (33 percent) of health care leaders surveyed would rate their system integration as excellent.
2. Data quality and interoperability
Being able to effectively manage large volumes of data matters because it has a significant impact on data interoperability. If the data being accessed to target patient interventions or assess quality improvement, are not accurate or cannot be trusted, it does little to further the goals of value-based care or meet compliance requirements.
Unfortunately, 40 percent of providers and half of payers surveyed cited data quality issues as a top challenge to integrating data across systems and gaining a full picture of patient health.
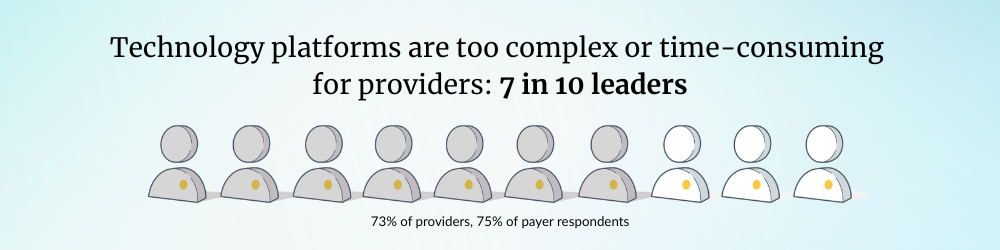
3. Complexity of technology platforms
The complexity of data management technology remains a top challenge for value-based care organizations.
To address data quality issues both payers and providers need to standardize data formats across systems and ensure reliable data integration for better accuracy and outcomes. But that sounds easier in theory than in practice.
Seven in 10 leaders say technology platforms are too complex or time-consuming for providers to use technology effectively. This creates a huge barrier to provider adoption, jeopardizing value-based care goals.
4. Data security and privacy
Finally, underneath all of the potential data required to drive measurable improvements in health care quality (and at a lower cost) is the flipside: concerns about data security and privacy are increasing.
- Over half (55 percent of providers and 56 percent of payers) of leaders surveyed rank data security as one of their top challenges.
- Twenty-four percent of providers and a third of payers (34 percent) reported suffering major cybersecurity incidents in the past year.
For data to be useful, it has to also be protected, safeguarding the organizational reputation, financial sustainability, and patient privacy.
The promise of AI: Unlocking the potential of your data
Advances in health care AI are creating significant opportunities for organizations to bridge the data gap and take advantage of the large volumes of data they collect. Providers and payers both recognize the value of artificial intelligence. More than 9 in 10 providers and nearly as many payers see positive impacts from AI on operational efficiency, predictive modeling, and the overall costs of administering value-based care models.
Using AI to perform critical data management tasks not only saves hours of staff time by doing the work of integrating data from disparate sources, but it can also produce highly relevant clinical insights and automate workflows.
- Aggregate and ingest data: AI can manage and ingest large volumes of data from disparate sources and formats. Then normalize structured and unstructured clinical data from sources like EHRs, HIEs, claims data, lab results, etc. to then be mined for insights.
- Develop clinical insights for value-based care programs: AI-powered technology can plays a crucial role in value-based care programs by delivering streamlined, actionable clinical insights into a provider workflow. These insights support patient targeting, pre-visit reviews, and post-visit documentation validation. By ensuring insights are both relevant, accurate and easy to use, AI solutions enhance provider engagement and adoption, ultimately enabling organizations to close care gaps, improve outcomes, and more effectively achieve value-based care goals.
- Enhance data security and compliance: With new technologies comes increased vulnerabilities. Technology vendors that incorporate HITRUST requirements with real-time monitoring, encryption, and automated breach notification protocols can improve the security of data, protecting the organization’s reputation and patient privacy while leaning into advanced technologies.
Health care organizations know that the road ahead must lead to lower costs and better outcomes. Still, achieving the goals of value-based care requires significant work, work that is constrained by the realities all health care organizations face.
Fortunately, advances in AI can be the missing link to take data strategies from promise to proof. Addressing complexity and the needs of interoperability head on by enhancing data management, data quality, and security is non-negotiable in advancing value-based care and the potential for improved financial outcomes and elevated standards of patient care.
Join our webinar, The Tipping Point in Value-Based Care, on Thursday, October 9 to hear how industry leaders are navigating this moment, and what steps you can take to accelerate performance in risk, quality, and clinical outcomes.

