The three-day annual event included four preconference workshops and two days of general and concurrent track sessions that addressed risk adjustment strategies, quality, compliance/regulatory updates, payer/provider alignment, and how to achieve health equity and address the social determinants of health (SDoH) for the aging population. Below are highlights from select sessions.
Why Medicare members leave your plan – even if they are satisfied

We heard from eight seniors who shared their experiences with Medicare and Medicare Advantage (MA) and what would cause them to switch plans.
The good news: All the patient focus panelists said they were satisfied with their plans in 2022. The bad news: Half of them still plan to shop around for another plan.
RELATED: Live from RISE West 2022: Day one
The discussion, moderated by Shannon O’Connell, senior manager, Engagys, revealed that convenience is a huge factor when choosing a plan. That means a network that includes their current (and nearby) doctors, better over-the-counter benefits, and an attractive rewards program. One panelist who is healthy and plans to travel in 2023 said he may leave his MA plan that he likes and enroll in traditional Medicare in case he gets sick when he’s away and isn’t near his network providers.
Among the panelists who will shop around for a new plan during AEP was a senior who has been with his current plan for five years. But he looks at his options every year. “It’s like automobile insurance,” he said. “When it’s renewal time, I start snooping. Maybe the snooping will result in more bang for my buck and if does, the search was fruitful. And if it’s not, I stay where I’m at.”
Regulatory and legislative activity to keep on your radar

The RISE Policy Committee discussed the spill-over effects of the Inflation Reduction Act, as well as pressing policy issues that impact health plans and risk-bearing providers in the managed care, Affordable Care Act (ACA, and commercial sectors. Among the concerns:
- The fact that Medicare finally can negotiate the price of certain drugs could lead to cost-shifting from one drug to another and cost-shifting to the commercial market, said Mike Adelberg, leader of Faegre Drinker Consulting’s health care provider and plans practice
- Medicare beneficiaries may have more cash available to them since the Inflation Reduction Act caps the amount they pay out of pocket for prescription drugs. But Adelberg noted that it’s clear from the patient focus panel that while it may make members satisfied, they may only be satisfied for one year. “It’s transitory satisfaction,” he said. “After a year, it’s an expectation. What do you do for them next year?”
- Mikal Sutton, managing director, Medicaid policy, Blue Cross Blue Shield Association, said she is concerned with the Medicaid redeterminations at the end of and unwinding of the COVID-10 public health emergency (PHE). Studies indicate that 15 million people and five to seven million children could lose their coverage once the PHE ends. While the PHE is scheduled to end in October, Sutton said all signs point to it being extended through mid-January, after the midterm elections. The Centers for Medicare & Medicaid Services is not taking the issue lightly and has been working with multiple stakeholders, including managed care organizations, to come up with comprehensive guidance for states.
Risk adjustment litigation and risk areas for MA plans, vendors, and downstream entities
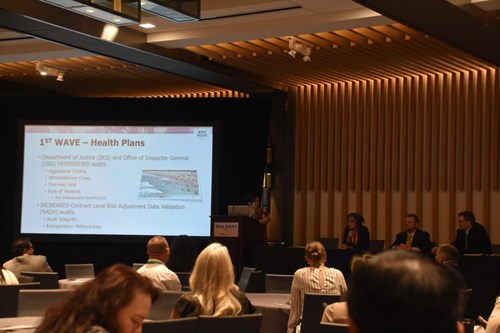
Panelists explained the current state of risk adjustment litigation by describing MA as an ocean, comprised of
- Waves or the challenges, obstacles, problems in the MA risk adjustment system (including various types of government oversight and enforcement actions)
- Boats/surfers/swimmers or MAOs/providers/vendors that participate in the MA RA system
- Lifeguards or individuals, and entities that monitor the MA RA program and watch for problems
- Sharks, crabs, and other sea creates are participants in the program, some of whom present dangers
The first wave, explained Mary Inman, partner, Constantine Cannon, involved Department of Justice cases for risk adjustment fraud against MA plans. All but one of the cases came from whistleblowers. Her advice: Save a lot of heartache and listen to whistleblowers when they try to tell you sharks are circling.

Second waves involved providers, the third wave focused on vendors and consultants, and the fourth wave was a deeper dive into Office of Inspector General audits.
Inman, Ed Baker, of counsel, Constantine Cannon, and Stephen D. Bittinger, partner, K&L Gates, LLP, said that health plans need to pay attention to future potential liability for improper denials and proper documentation, assessment/revision of chart review programs, and upstream liability. Providers also need to pay attention to proper documentation and audits and incorporate lessons into their compliance plans.
What’s next? Speakers said to expect a focus on the role of private equity, value-based contracts, upstream liability, and COVID-19 relief-related fraud.
How one partnership helped to close HEDIS® care gaps and improve member experience measures

Julianne Eckert, senior director, clinical quality programs, Clover Health, and Archana Mahimkar, senior director, clinical quality improvement and safety, Walgreens Health, discussed the innovative and collaborative approach Walgreens Health and Clover Health took to improve the lives of MA members in New Jersey.
Clover Health serves a large population who live in socially disadvantaged neighborhoods. Seventy-two percent of their MA members have been diagnosed with two more chronic conditions and the area deprivation index scores are much higher among Clover Health members compared to New Jersey as a whole. They partnered with Walgreens Health to provide digital and in-person wrap-around services via Health Care Corners that offer access to personalized, clinical expertise, a tech bar where patients can receive continuing education, and one-on-one visits with a health adviser.
There are more than 25 Walgreens Health Corners available to members who live in the most populated counties. “Our goal is to make care easy and convenient and bring care to members rather than members seeking care and travel and we want to target areas of the highest concentrations of our members,” said Eckert.
For Walgreens Health, the collaboration is a “significant way to build sustainable relationships with Clover members in the community where the member lives,” Mahimkar said.
The collaboration led to a return that was greater than expected:
- In one year, the partnership saw ~20 percent of its controlling high blood pressure HEDIS hybrid members demoninator had Health Corner blood pressure checks
- The Walgreens Health Corners Customer Satisfaction rate of 97.2 percent for CY2022 exceeded the 80 percent target
- In 2022, health advisors have had 54,599 conversations with members within Health Corners
- More than 6,000 of these conversations resulted in care gap closure services
- An improvement in Star ratings from 3 to 3.5
The Health Advisors at Walgreens Health became “Clover Health ambassadors,” according to Eckert. “They knew our benefits, they knew our members, and they knew how to manage them and help us identify unknown barriers to care and needs. They were able to address urgent health conditions and address with the doctor, Clover teams, or the hospital for treatment,” she said.
The partnership has led to providing members with offerings that address prevention, treatment, and wellness. The speakers encouraged attendees to think about health care differently to make it sustainable and easier to navigate. Doctors are overwhelmed so it makes sense to have the Walgreens Health Corner staff provide screening and other basic care and alert clinicians so they can make the best clinical decisión for members.
Mahimkar said the next step is scaling the member-care advisor partnership model and building a multi-modual approach to care including onsite, in-home, and whole-person care /
Why attendees come year after year

It was our biggest conference to date with more than 650 participants. Attendees left with new connections, a wealth of knowledge, and actionable steps to take back to their organizations. Here’s what a couple of attendees had to say:
“RISE West does a great job of weaving quality and SDoH together with risk adjustment,” said Anna Basevich, vice president of enterprise partnerships, Arcadia. “HCC coding is an inherently actuarial topic, but RISE highlights presenters who’ve grappled with the challenge of assembling accurate and comprehensive patient records to ensure both appropriate reimbursements and the right information to allow care teams to support their populations effectively. I was excited to see discussion around SDoH as this area presents much promise for health care organizations to understand their patients and engage them with the interventions that account for barriers to care that have traditionally held back progress.”
Enam Noor, CEO, and founder, Insightin Health, said that by attending the conference, health plans can better consider their role in stewarding their members’ wellbeing over time and investing in a data-driven, omnichannel engagement approach that offers deeper insights into creating personalized health care journeys for members. “By understanding the health of members and the challenges they face as well as overcoming obstacles to proper communication and care coordination, health plans will be better positioned to address member needs and improve satisfaction,” he said.
