More than 250 participants are gathered at Capitol Hill for the RISE-Aligning for Health inaugural Social Determinants of Health (SDoH) Policy Forum this week to engage with government leaders about policies that address the non-medical factors that influence health outcomes and funding opportunities to increase coordination and improve well-being and whole-person care. Check back frequently as we post about the event throughout the next two days.
Today’s sessions featured keynotes from White House, Centers for Medicare & Medicaid Services (CMS), and Centers for Disease Control and Prevention (CDC) officials. Here’s a sampling of what we’ve learned so far:
Aligning for Health state of the industry report

Krista Drobac, co-chair, Aligning for Health, kicked off the conference Tuesday morning with a state of the industry address. She noted that so far during the 117th Congress, lawmakers have introduced approximately 243 bills focused on SDoH, including funding for programs and to improve SDoH coordination. Seventy-nine bills are focused on health disparities/equity and 99 bills address maternal and infant health.
There has been a growing interest in SDoH on Capitol Hill, she said. Congressional leaders have focused on increasing funding or expanding eligibility for federal programs that address SDoH, as well as legislation to promote cross-sector SDoH coordination and legislation to advance health equity.
She encouraged attendees to network with those who are outside their sectors. Relationship building is vital to advance the cause, Drobac said. “We are trying to address the whole person. We live horizontally but all our programs are vertical. Budgets and reporting align vertically but people live across all these programs,” she said, stressing the importance of thinking about the people who benefit from these programs and the user experience.
Keynote: Dr. Sandra Ford on current White House initiatives and future plans

Addressing SDoH and advancing health equity is a priority of the Biden administration, said Dr. Sandra E. Ford, special assistant to the President for public health and science, White House Domestic Policy Council.
She described health equity as the opportunity to live your best life, irrespective of your social circumstances. It includes a person’s length of life; quality of life; rates of disease, disability, and death; severity of disease; and access to care. While health equity is advanced by addressing SDoH, they aren’t the same.
There are many disparities in health equity, including severity of disease and ability to access care. The pandemic, she said, changed the game in equity. People were shocked by the differences in hospitalizations and deaths related to COVID and which individuals were more likely to survive based on their ethnicity. But no one at the county and state level and those in the field were shocked, she said. Health equity is generational and not new. But the pandemic numbers were so dramatic that people had to sit up and acknowledge the problem.
The impact on homelessness was especially significant, Dr. Ford said. The overall infection rates among those who were homeless were 61 percent higher than the general population. The elderly and those with underlying chronic illnesses were particularly vulnerable. Fewer social services were available, there were closings of 220(h) funded housing, more food insecurity, and more job loss, which led to move evictions and more homelessness but a decreased access to shelters as they closed or had limited space. Those who are homeless have a 30-year less life expectancy than those who have secure housing. “If their life expectancy was 80, they now have until 50 through no fault of their own other than not having a roof over their heads,” she said.
To address this, the American Rescue Plan provided $1.9 trillion that included funds for housing, food insecurity, mental health, Medicare, Medicaid, and CHIP. The plan included 70,000 emergency housing vouchers, funding for unhoused families, and money for the Emergency Rental Assistance. Vice President Harris conducted the National Conference on Ending Homelessness in July that focused on a whole-of-government response. It’s not just an issue for HHS and HUD, Dr. Ford said. “Everyone has a stake in this,” she said.
Since taking office, President Biden has also signed dozens of executive orders that address SDoH and health equity. These include orders for racial equity and support for underserved communities; an equitable pandemic response and recovery and the establishment of the health equity task force; strengthening Medicaid and the Affordable Care Act; expanding access to care and treatments for COVID-19, and diversity, equity, inclusion; and accessibility in the federal workforce.
As for the future, the White House’s action plan includes a whole-of-government approach to link hospital systems, public health, and social services. This includes 35 federal agencies and departments and 22 external stakeholder organizations. Dr. Ford noted potential policy levers to address SDoH are via:
- Alignment of data use and privacy policies
- Blending and braiding of funds to create conditions that optimize health and create healthy and resilient communities
- Support for backbone organizations
Keynote: CMS policy developments

Ellen-Marie Whelan, NP, Ph.D., chief population health officer, Center for Medicaid and CHIP Services, CMS, discussed the agency’s commitment to address SDoH, health equity, and maternal health.
Whelan, who also serves as senior advisor, Center for Medicare and Medicaid Innovation, CMS, acknowledged that it has only been in recent years that the agency began to shift from paying for quantity of services to quality and improvements in outcomes. Twenty years ago, she said, the Institute of Medicine estimated that 100,000 people each year were dying from medical errors. Yet CMS continued to pay without regard to quality, outcome, or cost of care. It was only in 2007 that CMS made a policy decision not to pay for never-events, such as surgery on the wrong body part.
“That means 15 years ago if a physician accidentally cut off the wrong leg, CMS was paying for it without the regard of outcomes. Since then, we continue to look at ways of reimbursement based on improved patient outcomes…CMS now understands to improve outcomes, you need to provide holistic care and take into account the social determinants of health. The fact that CMS thinks about that and changing payment based on that is truly remarkable,” she said, adding that the agency is better committed to understanding and addressing disparities and to promote equity.
One of the first executive orders signed by President Biden was to advance racial equity. To help achieve this, CMS is promoting health equity, working to level the health care level. And it is looking at what it already has in its toolkit to better address SDoH. “No American should be left out or left on sidelines on affordable coverage and quality healthcare,” she said. “We realize we have a role in promoting health equity, what is the responsibility we should have as payers for health care? Some tools we have are improving and expanding coverage…But we need to make sure it’s quality coverage.”
She noted the strides CMS has made in quality by tracking hospital inpatient quality measures to address health disparities and three equity-focused measures. These measures assess a hospital's commitment to create a culture of equity, capture activities for strategic planning, leadership engagement, and quality improvements. Hospitals have to attest that equity is a strategic priority and data is being analyzed for disparities. “These are things that CMS wasn’t looking at before,” she said.
Whelan said the agency is also reaching out to the public for feedback on future plans, including a new health equity index in Medicare Advantage and a finalized health equity adjustment in the Medicare Shared Savings ACO program, which reward excellent care for serving underserved populations across Medicare.
Keynote: CDC on expanding community capacity to advance whole person health



Dr. Karen Hacker, director, National Center for Chronic Disease Prevention and Health Promotion, CDC, provided an overview of how the center worked to advance its mission to help people and communities prevent chronic diseases and promote health and wellness for all.
The center, she said, has targeted SDoH in various ways, including food and nutrition security, a tobacco-free policy, social connectedness, and community-clinical linkages. As a result of their efforts, more than 2.9 million people have better access to healthy foods and beverages, over 322,000 people have benefited from smoke-free and tobacco-free interventions, 1.4 million people have more opportunities to be physically active and more than 830,000 people have access to local chronic disease programs that are linked to clinics.
"We see social determinants underneath an umbrella as a strategy and activities to get use closer to health equity," she said.
To fast-track improvements in health and social outcomes among populations experiencing health disparities and inequities, grants have been given to cities, counties, districts, states, and tribes. This year the agency is evaluating 14 communities for needs and next year intends to focus on the health care system.
She also discussed the progress of The Gravity Project, which launched in May 2019, and brought together more than 2,000 participants from across the health and human services ecosystem. The project aims to develop data and exchange standards to represent SDoH data documented in electronic health records across four clinical activities: screening, diagnosis, goal setting, and interventions.
To help health care systems address SDoH, Dr. Hacker said the agency is partnering with public health departments and community-based organizations, investing in addressing social needs and SDoH, supporting health promoting policies, and screening for social needs and SDoH.
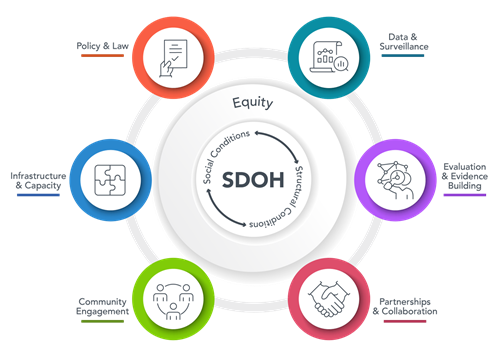
The CDC's SDoH framework is listed below, with health equity at the center.
To begin, the CDC has concentrated its efforts on five areas to address SDoH: Food and nutrition security, tobacco-free policy, built environment, social connectedness, and community-clinic linkages. "Chronic disease is so linked to these opportunities, particularly for COVID there was a disproportionate impact on various communities across the nation," Hacker said, adding that the CDC is trying to work with multisector partnerships within communities to develop their own strategies to help those make best decisions in care.
"No single entity can do this work on its own," she said. "Cross-sector partnership is foundational to moving forward And we need to align public health and social services to facilitate moving forward," she said.
Shout out to our volunteers at the food packing EVENT


Before the conference began, dozens of attendees joined us Monday afternoon for a food packing event in partnership with U.S. Hunger U.S. Hunger (Feeding Children Everywhere). Volunteers packed 15,684 meals that were sent to the Capital Area Food Bank. Special thanks to all the attendees who took time out of their day packing the meals as part of a commitment to make a difference in the local community.
