The second day of The RISE Summit on Social Determinants of Health featured discussions on access to data and funding streams for SDoH sustainability, innovations at the state level, opportunities to address SDoH for Medicare Advantage members, a fireside chat on the reality of being a patient and consumer in the health care system, and more. Here is a recap of our biggest takeaways.
We kicked off our final day of the summit with the presentation of the 2024 Health Care Hero award, which acknowledges an individual’s effort to make a significant impact on the lives of underserved populations through health care and/or social services interventions, and through superior example of the RISE mission to promote health equity among all patients.

This year’s recipient is Dr. Kimberlee Etheridge, primary care provider and assistant professor, Meharry Medical College; sr. VP health equity and diversity initiatives, ASTHO.
Dr. Etheridge, who was selected out of a field of 59 nominees, was chosen for her work as an adolescent provider for the pediatric department at Meharry Medical College; her work teaching first-year medical students; her involvement in her community providing education and services to pregnant women and recently delivered families to increase infant and maternal vitality; and her work promoting health equity on the national level with the Association of State and Territorial Health Officials (ASTHO).
RELATED: Dr. Kimberlee Etheridge named RISE’s 2024 Health Care Hero
While accepting the award, Dr. Etheridge said she was honored and shared how growing up in world that told her she couldn’t, drove her to show just how much she could– and did. “I’ve lived my life with intention and dedication to a purpose and never losing site of who my true boss is,” she said. “And it’s not the person who signs my paycheck but the person who gives me peace knowing I have made a difference to somebody. This work is hard, but it is not impossible. We need to remind ourselves why we do what we do.”
Access to Data and Funding Streams as the Backbone to SDoH Sustainability
We heard from an eye-opening panel of industry leaders this morning as they discussed the sustainability of SDoH programs through innovative funding and data access.

Throughout their conversation, the panel brought three clear issues to attention that are barriers to addressing SDoH:
1. The questions asked in SDoH screening need to be expanded.
“We need to ask ourselves- are there questions we put in the EHR, questions I’ve fought so hard for, are those actually the right questions? Will they get us there?” said DeAnna Minus-Vincent, founder and managing partner, The Outcomes Architect, stressing the need for screening to be more of a conversation between the doctor and patient.
2. Incentives are misaligned.
“The incentives are all misaligned, that’s the real root cause,” said Zeev Neuwirth, M.D., MHA, internal medicine physician, author, “Beyond the Walls”, podcast host, 'Creating a New Healthcare'. “The evidence is that 80 percent of medicine should be going to SDoH. Until we redirect funds and incentives and payment to the 80 percent, we’re just whistling in the wind.”
3. Focus needs to shift to fixing the problem rather than predicting it.
“Everything is wrong about this picture,” said Esther Dyson, founder, Wellville. “We need to be investing in maintenance and not repair. Our human capital is worth more than all the physical infrastructure.”
Innovation at the State Level
We also heard from a panel of leaders on the ground in North Carolina who shared insights around their state-level initiatives, including the operationalizing of public/private partnerships and details of the coordinated care technology platform, reimbursement, metrics, and sustainability.
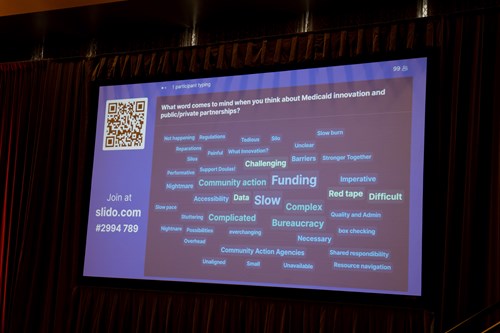
Looking for attendee feedback, the panel asked attendees to participate in an interactive Word Cloud activity, where they submitted words that came to mind when they thought about Medicaid innovation and public/private partnership.
The most common words: Slow, complex, funding, difficult, clunky, complicated; bureaucracy; community action; data; barriers; red tape.
While discussing their biggest takeaways and best practices, the panelists drove home the importance of looking at not only how you are capturing information but how you are evaluating it. “We all have data, but data is nothing without evaluation,” said Tim Driscoll, assistant director of service coordination, Veterans Services of the Carolinas. “Data can inform organizational decisions, but if you don’t have evaluation showing it’s working, there’s no sustainability.”

Opportunities in Addressing SDoH for Medicare Advantage Members
Another key focus today was how Medicare Advantage (MA) plans are addressing SDoH for their members and communities. A panel of experts shared their insights and examples of how their organizations are addressing SDoH, and they also dove into the Health Equity Index (HEI) and Social Needs Screening and Intervention (SNS-E) measures to improve health care access and outcomes for plan members, especially those with specific social risk factors.
“This Health Equity Index is over 10 years, meaning it’s across administrations, and that’s important because from a sustainability standpoint, that means CMS is seeing this in the long term,” said Ana Ana Handshuh, principal, CAT5 Strategies, noting that addressing SDoH came into play during our last administration under Seema Verma and continued with the current administration under Chiquita Brooks-LaSure. “What that tells us is it shouldn’t matter what your politics are, these issues are real. In order to improve health care in our country, we’re going to have to get very serious about addressing SDoH and health equity.”

A Look Into a Patient’s Journey in “The System”
Charlotte Safrit, a breast cancer survivor and community organizer, sat down with Conference Co-Chair Ellen Fink-Samnick to share with us a vulnerable look at her story as a patient in the health care system.
She spoke up for women and mothers, like herself, who have had to fight for imaging and were inaccurately told that they could not receive imaging while breastfeeding.
“My breast cancer support group is a small, intimate group, very hyperlocal, with about 40 women” said Safrit. “Yet, I’ve had 10 women join who had to fight for their mammogram due to their breastfeeding, and by the time they finally got it their cancer was in advanced stages.”
Safrit, who discovered that women can in fact receive a mammogram while breastfeeding through her own research of advice from La Leche League and the American Radiological Society, is on a mission to spread the word throughout health systems in hopes of saving other women’s lives.
When asked what the single biggest takeaway is, Safrit said it’s for patients to be heard.
“Listen to your patients. Listen to them,” she said. “Every person has a story, and I think all of us, whether we be medical professionals or patients, we have something to give and learn from one another, and unless were listening to one another we cannot come up with individualized treatments for patients. We have a beautiful opportunity to rebuild the system and turn it into a living organism that responds to the patients’ needs and with all of your inputs and expertise, hopefully we can just save more lives to make it a better health care system for all of us.”
