Multiple versions of Interim Final Rules and Final Rules have been released in 2020, all related at least somewhat to COVID-19’s impact on Star Ratings. Health plans often interpret the rules differently. In this piece, Rex Wallace of Rex Wallace Consulting and Mick Twomey of Hyperlift, help clarify the rules.

If you’ve ever tried to learn a foreign language as an adult, you know how it feels to read and try to fully comprehend the Interim Final Rules in 2020 from the Centers for Medicare & Medicaid Services (CMS). Unfortunately, the consequences of misinterpreting these rules will most likely have a larger impact than accidentally ordering the wrong appetizer at that restaurant in Tokyo.
Multiple versions of Interim Final Rules and Final Rules have been released in 2020, all related at least somewhat to COVID-19’s impact on Star Ratings. And as we (RWC and Hyperlift) have collaborated on the impact these rules will have on 2022 Stars, we realized that different health plans are interpreting these rules differently. So we decided to attempt to bring some clarity to these rules, with the assistance of some feedback directly from CMS.
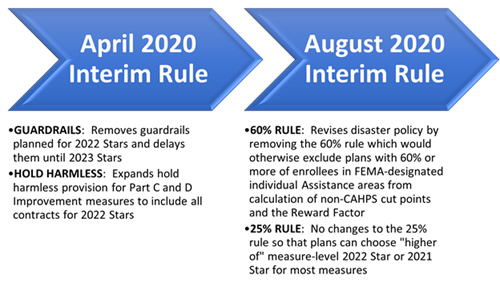
We will focus on the two Interim Final Rules, published in April and August. The image below captures the four high-level summary points of the rules. However, as they say, “the devil is in the details,” and we will spend the rest of the article helping you see through the fog.
High-level summary of the 2020 Interim Rules’ impact on 2022 Stars
Guardrails
To increase the predictability of cut points, CMS previously announced it would implement guardrails for 2022 Stars for measures that have been in the Star Ratings program more than three years. The guardrails would prevent non-CAHPS measures from increasing or decreasing more than 5 percentage points from one year to the next. As a result of the likelihood that COVID-19 could cause at least some measures to decline significantly, CMS has decided to delay the implementation of these guardrails until 2023 Stars so that cut points can change more than 5 percentage points to accurately reflect industry performance and not penalize health plans.
Hold harmless
Typically, for plans with an overall Star Rating of 4+ Stars, if their overall Star Rating declines when adding in the improvement measures, then the improvement measures are excluded from the calculation. Thus, already-high-performing plans are not penalized for not improving significantly from one year to the next.
In the Interim Final Rule in April, because performance is expected to decline for plans across the entire nation, CMS expanded this hold harmless provision to include all plans, regardless of their rating. These changes are for 2022 Stars only. When this was initially communicated, it seemed clear enough. However, the newest Interim Final Rule in August seems to have muddied the water. More on that below.
60 percent rule
In August, CMS released a new Interim Final Rule addressing the disaster policy. CMS realized that unless it changed the existing rules, it would not have enough contracts to reliably calculate measure-level cut points for non-CAHPS measures for 2022 Stars. In fact, ~98 percent of plans would be excluded from calculations. Thus, CMS would be unable to calculate 2022 Stars and, subsequently, distribute 2023 Quality Bonus Payments (QBPs).
For 2022 Stars, CMS adjusted the disaster policy by removing the 60 percent rule, which excludes plans with 60 percent or more of their enrollees living in FEMA-designated Individual Assistance areas from calculation of non-CAHPS measure-level cut points and calculation of the Reward Factor. As a result of this change, CMS will now be able to calculate 2022 Stars and distribute 2023 QBPs.
25 percent rule
The 25 percent rule allows contracts that have 25 percent or more of their enrollees living in FEMA-designated Individual Assistance areas to receive their previous year’s measure-level Star Ratings and measure scores for most measures if they are higher than the current year. CMS made it clear that it is not revising the 25 percent rule. Plans will still be allowed to pick the “higher of” Star Rating between 2021 Stars and 2022 Stars (which actually includes performance as far back as 2018 for HEDIS and CAHPS) for all measures except the Improvement measures and the Call Center measures.
An important nuance of these changes is that any measure that receives the previous year’s Star Rating (because it was higher than the current year’s Star Rating for that measure) is excluded from the Improvement measure calculations. Also, contracts must have data for at least half of the attainment measures used to calculate the Part C or D Improvement measure to receive a Star Rating for each of those measures.
This is important. It means that plans whose 2021 Stars are re-applied for multiple measures need to understand the impact of those measures no longer being included in the Improvement measure calculation. Most plans, we believe, will still benefit from this, as being able to receive the “higher of” the 2021 Star or 2022 Star for most measures should result in higher Star Ratings for many of those measures. This should offset any potential disadvantages of excluding these measures from the Improvement measures.
Of course, brand new plans will not benefit from the 25 percent rule, as they will have no 2021 Stars. They will be scored solely on their 2022 Stars.
What to do
COVID-19 has wreaked havoc in 2020, and it continues to create much uncertainty as we prepare to enter 2021. However, if health plans understand the new rules, dig into their data and can predict the impact of the rules, and strategize accordingly in what remains of 2020, they potentially stand to benefit significantly as a result of COVID-19, albeit perhaps just for a single year.
A potential pitfall looms before us. There is industry concern that the ability for every plan to choose the “higher of” Star Rating for most every measure will create a one-year surge in plans achieving 4 Stars. Some plans will surpass the 4-Star threshold for 2022 Stars and receive unexpected–and perhaps unearned–QBPs. This newfound revenue will positively impact member benefits and premiums in 2023. However, if those plans are unable to sustain a 4+ Star Rating, that revenue goes away in 2024 and members receive reduced benefits and increased premiums, thereby creating a negative experience that will be reflected in member experience measures. Thus, plans’ Star Ratings will potentially fall even more.
Plans need to strategize now and throughout 2021 on how not to regress back to the mean for 2023 Stars. They need to engage and inform their Executive Steering Committees about the importance of improving now. Securing funding to launch critical initiatives. Asking hard questions around every domain.
- Which measures can we reach “significant improvement” in?
- How will our improvement measures be impacted knowing that measures with higher 2021 Stars will not be included in their calculations?
- Are we utilizing text outreach to improve Medication Adherence?
- Are we capturing the voice of the customer and socializing it within the organization?
- Are we incenting members to take healthy actions?
- Are we executing flawlessly all of those operational activities in our control?
- Are we providing accurate, real-time, actionable data that is tied to robust incentives we deliver to our provider partners via a collaborative engagement?
Summary
We hope this helped clarify the Interim Final Rules for you. Below is a summary of the highlights. Good luck with 2022 Stars.
*If you’d like to run your numbers through our “Better Of Model,” please send a request to mick.twomey@hyperlift.com and he will send you a model for you to use on your contract(s).
Highlights
- The “higher of” rule applies to all Part C and D measures (outside of the QI measures and Call Center measures). Specifically, both CAHPS and HEDIS are included also.
- The “higher of” determination will be done by CMS automatically after all of the Stars 2022 scores are submitted and will compare the Star Ratings (not measure scores) between Stars 2021 and Stars 2022 (after cut points have been applied to determine the associated Star Rating for each measure in Stars 2022). If the Star Rating is the same in both years, the Star Rating and the measure score from the most recent year are used.
- The cut points for Stars 2022 will be determined using all plans and measures, including the scores for measures in plans that don’t end up getting used due to the “better of” determination. Normally, contracts with 60 percent or more enrollees living in an Individual Assistance area are excluded from the measure-level cut point calculations. However, CMS finalized an emergency rule removing the 60 percent rule for cut point calculations for non-CAHPS measures and calculating the cut points based on all contracts that qualify for a particular measure.
- If the “higher of” results in the use of a Star rating from 2021, that measure will be excluded from the Quality Improvement measure rating calculation.
- The starting point for the Stars 2022 QI calculation will be the Stars 2021 scores for all eligible measures that use their Stars 2022 results. The QI measure will compare 2022 scores with 2021 scores.
- The Hold Harmless provision that usually applies to only 4-Star plans, will be applied to ALL plans for Stars 2022.
- Contracts must have data for at least half of the attainment measures used to calculate the Part C or Part D improvement measure to be eligible to receive a rating in that improvement measure.
About the authors
Rex Wallace is the founder and principal of Rex Wallace Consulting, LLC, a firm that specializes in improving Star Ratings for Medicare Advantage health plans. Rex assesses plans and guides them in the development and implementation of industry-leading strategies to drive material Quality Improvement.
Mick Twomey is the president and chief operating officer at Hyperlift, Inc. Hyperlift specializes in providing data-driven strategic planning deliverables and monthly Stars Performance Scorecards and Dashboards to provide Stars teams with transparent, actionable insights using predictive analytics and compelling data visualization solutions.
