For the fifth installment of our semi-regular series that recommends articles, white papers, or issue briefs of importance to RISE members, we suggest United Hospital Fund of New York’s white paper Complex Construction: A Framework for Building Clinical-Community Partnerships to Address Social Determinants of Health. The paper provides an insightful look into the hurdles that organizations face when they try to leverage the resources of community-based organizations to meet the social determinants of health needs of their patients in a medical setting.
The independent, nonprofit organization collaborated on the project with the New York City Population Health Improvement Program, with funding from the New York State Department of Health. During the year-long project, the United Hospital Fund (UHF) worked with two federally qualified health centers to understand and document the process of screening for social needs in primary care. It also developed relationships with community-based organizations (CBOs) to design and implement processes to facilitate referrals and follow-up on patients.
UHF’s paper focuses on the complexities of building a working referral network that community providers can use in the area of social determinants of health (SDoH). It suggests concrete and crucial elements in executing an SDoH strategy in a logical manner. These elements, if taken one at a time, will help health care organizations tackle a strategy with the right resources and planning. Here are the core take-away ideas:
- There is no single standardized/interoperable approach to information technology that supports tracking social needs in primary care practice settings
- Increased screening is likely to increase demand for CBO services, which may not have the bandwidth or resources to scale up
- Payment resources for current value-based care are not adequate to cover investments needed to respond to social needs
- Organizations must evaluate the effectiveness of new SDoH programs
When viewed from this vantage point, the first point underscores the gap in technologies currently available in the health care industry. The inventory and capacity issues cited reflect the nature of the CBOs as often underfunded and under-resourced community service agencies. The single biggest obstacle, however, is the third bullet: a lack of funding to drive the whole SDoH resourcing dynamic. Without adequate, large scale funding, there is a dearth of experience from which to construct ROI analyses.
While there are many public conferences convening about SDoH, we have yet to see anything that provides a unifying and integrating framework for building out SDoH strategies that is as concise and useful as the recommendations offered in the UHF paper. The brief does an admirable job of spelling out the underlying details of what needs to be done to execute SDoH initiatives. It provides a highly useful framework for the as-yet-to-be-built collaborations with CBOs.
UHF finds that:
- There is a growing literature base that documents the impact of social factors on health
- People without resources, particularly those who experience homelessness, food insecurity, unemployment, violence, etc., are disproportionately poor, and these conditions have a larger impact on a person’s health than the medical care they receive
- Health care providers, payers, and policymakers must systematically identify people who need help with SDoH referrals
- Primary care providers are a trusted source to address health needs, but there is no system in place to support the need for a referral and feedback loop
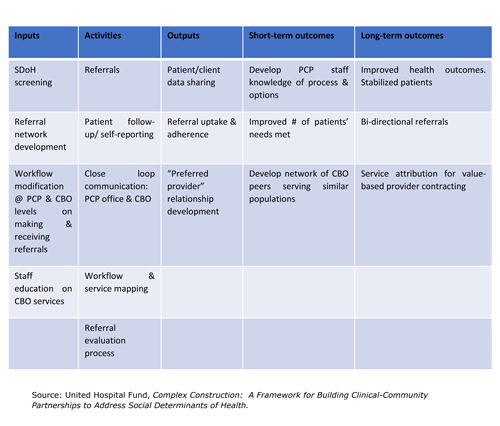
A look at the framework
Primary Care – Community Partnership Framework Logic Model

RISE’s view
In our view, the work laid out in this paper is extremely useful as a starting place. However, RISE also believes that the major missing element is the funding source that would enable the system to coalesce and blossom. We believe that some Medicare Advantage Special Needs Plans and some Medicaid managed care health plans can make funding available depending upon state funding restrictions.
The whole notion of accountable care provided by managed care plans under contract with government health agencies is founded upon coming up with creative solutions to health care quality and spending issues while operating on an at-risk basis. If managed care plans became the third parties to the provider/CBO collaborations, it would allow for more resources and capabilities to address a framework as described in the paper:
- Technological platforms and tools for communications, resource databases, referral management, data collection / distribution, and case management tools
- Consensus building on standards, processes, and best practices dissemination
- Process and workflow standardization
RISE-affiliated health plans have developed certain core disciplines that would also help take this whole framework to another level: population health management, quality management, and revenue management within a capitation-based government health program model. We view the opportunity to serve as a catalyst for learning and knowledge transfer, best practice development, and partner/collaboration development.
It is for this reason that RISE aims to create a community of stakeholders dedicated to building this approach to enabling SDoH strategies to come about and flourish. Our expertise at community building among health care business partners, focused on “how to” knowledge transfer, is well-suited to bringing together a practical community of stakeholders, including providers, CBOs, technology companies, and managed care plans. Learn more about these collaborative efforts at the upcoming National Summit on Social Determinants of Health.
