Survey results show that Medicare Advantage Organizations recognize the critical need to improve communications with members and are finding new ways to create and manage the required Medicare marketing materials.
With the Centers for Medicare & Medicaid Services (CMS) planning to approve an expanding array of covered benefits, the market for Medicare Advantage plans is projected to grow from approximately 25 million enrollments to 34 million in five to six years. This is creating expanded opportunities to reach new members and positively impact their health and well-being. Perhaps in recognition of the increasingly important role of connecting with consumers in the current health care marketplace, Medicare Advantage Organizations (MAO) are responding to the critical need to improve communications with members by finding new ways to create and manage the required Medicare marketing materials.
According to a recent survey conducted by World Congress’ research arm, Health Value Institute, and commissioned by Messagepoint, the top four initiatives MAOs are investing in to improve the member experience are:
- Improving member onboarding
- Expanding plan types to better cater to member needs
- Improving the member servicing experience
- Making materials easier to understand
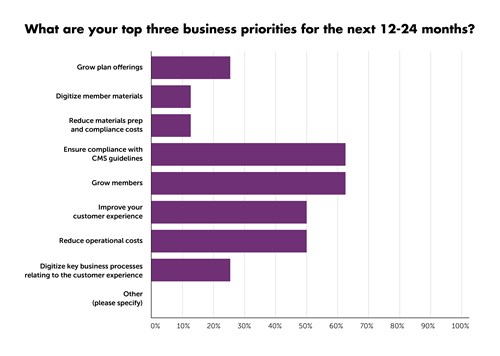
Respondents who participated in the survey work in operations, marketing management, product management/development and compliance for MAOs. All survey respondents play a role in member communications material preparation and management. While 100 percent of the respondents said improving the member experience is the overall priority for their organization, the three top areas of focus cited for the next 12-24 months are ensuring compliance with CMS goals, reducing operational costs, and growing members.
The respondents were split between several choices when it came to identifying the biggest challenges in meeting the goal of ensuring compliance with CMS requirements with the following concerns: manual processes for updates lead to human error and errata, the volume of plans under management, last minute changes by CMS, and weak quality assurance processes.
Respondents were asked about their approach to managing the following member materials:
- CMS-mandated materials for Medicare Advantage
- Prescription drug and Medicare-Medicaid Plans (ANOC, EOC, SB)
- Marketing and sales communications (Getting Started, BenHi, SBC, plan comparisons),
- Pre- and post-enrollment (directories, formulators, enrollment forms)
- Member servicing communications (correspondence, ID cards, 1095-B forms)
- Whether they are satisfied with the process
According to 50 percent of respondents, the top frustrations that affect their management of CMS-mandated materials include cost, the possibility of errata and fines. and no visible path to digital communications that would enhance both the workload and the member experience.
The survey highlights the fact that MAOs want to find ways to improve operational efficiency and accuracy to achieve the goal of a positive member experience. The top three areas relating to CMS-mandated materials health payers would like to improve are quality assurance, plan data management to ensure greater accuracy, and layout and content management processes to increase efficiency. MAOs employ a wide variety of approaches and solutions for managing plan materials. While some still heavily rely on manual processes and Microsoft Word or third-party service providers, most recognize the substantial benefits that can be gained by using software that is purpose-built for creating and managing these complex communications.
As a result of increased oversight and regulation by CMS, these organizations see the benefits of automation, but many struggle with justifying the expense. Furthermore, until recently, automation solutions with the capabilities needed to effectively handle these complex documents have not been commercially viable nor readily available. However, vendors in the Medicare marketing space, both software and print services, are working to provide solutions that will bring more capable and affordable automation options forward, allowing MAOs to leverage technology to meet their current and future requirements as they gain new members and grow their plans.
Finding ways to both cost-effectively automate and engage members with effective communications is a goal many health plans share. As companies evaluate technology solutions, it is important to research those that promote better member education and experience while at the same time streamline processes, reduce costs, and facilitate future member and plan growth to achieve these goals.
Messagepoint’s Healthcare Touchpoint Exchange is a purpose-built solution to streamline the creation and annual updates to your CMS compliance materials including Annual Notice of Change (ANOC), Evidence of Coverage (EOC), Summary of Benefit (SB) and other documents. Our unique approach enables customers to finish materials early with greater accuracy to meet their AEP goals. For more information, visit https://www.messagepoint.com/healthcare.
About the author
 Sohail Malik is vice president, health care solutions with Messagepoint, overseeing the Messagepoint Healthcare Touchpoint Exchange solution to ensure the support of the complex and ever-changing needs of health plans to scale and grow to meet market needs.
Sohail Malik is vice president, health care solutions with Messagepoint, overseeing the Messagepoint Healthcare Touchpoint Exchange solution to ensure the support of the complex and ever-changing needs of health plans to scale and grow to meet market needs.
He has more than 15 years experience in customer communications management and SaaS/Cloud-based digital transformation of highly regulated industries.
Malik has worked with some of the largest national health care organizations, Blues and smaller community plans to bring digitalization and process automation for client communications and helped them scale and grow their business.
