It’s become industry standard to code medical records to 95 percent. But would you be satisfied with receiving 95 percent of your paycheck each month? Or 95 percent of your retirement savings? Probably not. Yet many health plans currently accept a 95 percent coding accuracy rate.
Accuracy, efficiency, compliance—these are all qualities health plans aim to achieve in their risk adjustment programs. So, why is it that most plans only code medical records to 95 percent accuracy? Leaving even that 5 percent on the table could mean missing out on 25 percent+ of a chart’s potential value, not to mention the increased risk of being audited. In today’s challenging landscape of rising costs and growing compliance risk, 95 percent accuracy is no longer enough.
Second level reviews are an excellent way for health plans to improve coding accuracy, but many do not currently use this strategy. Perhaps this is because traditional programs have typically been lengthy and manual processes that require a full duplication of work. The introduction of AI and NLP, however, has transformed the second level review into a more efficient and effective process—one that can help ensure risk score accuracy, mitigate compliance issues, and ultimately improve patient care.
Training technology to work for you
Natural language processing (NLP) is a branch of AI that brings together linguistics, statistics, and machine learning to allow computers to understand text and spoken word, including unstructured data such as a provider’s handwritten notes on a patient chart. Without NLP prioritization, coders must manually comb through charts looking for this information, which can be a time consuming and cumbersome task.
By streamlining data input and validation, NLP can help plans achieve more accurate, complete diagnosis capture. But the technology is not a panacea in and of itself. The adage “garbage in, garbage out” helps explain the limitations of NLP in this context. In other words, NLP is only as good as the data used to train it. The more records that are used to train an NLP engine, the more it can learn and improve over time. Unfortunately, many NLP coding tools on the market today are trained by relatively small coding teams reviewing a limited number of medical records.
Using NLP to ‘look both ways’
In contrast, Episource’s NLP-targeted second level review engine, epiFinalCheck, has been trained by more than 3,500+ full-time coders on 11 million records each year. This includes a massive clinical taxonomy that maps conditions, labs, procedures, and medications via 2.5 million relationships. The tool is continuously refined to increase coding accuracy and “read” unstructured text, pick out keywords and phrases, and analyze them to determine whether a code is missing and needs to be added, or is noncompliant and needs to be deleted. As an extra layer of protection, human coders review each flagged discrepancy against both plan and Centers for Medicare & Medicaid Services’ (CMS) coding guidelines. This process of “looking both ways” is critical, but many NLP solutions take an upside-only view, leaving plans vulnerable to the compliance risk that comes with overcoding.
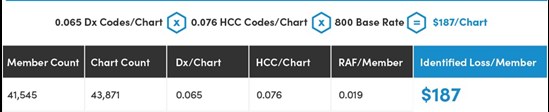
Incremental Dx codes HCCs & RAF per chart
When looking at a sample of 43,871 charts—all of which had already been coded, and many of which had undergone a multi-vendor, multi-level review—we identified 0.019 RAF increment per member that had likely been under-reimbursed. This translates to ~$187 per member per year (which could add up to millions across your entire population) in potential lost revenue that could be invested in enhancing programs and improving patient outcomes.
The real goal of increased accuracy: Improving patient outcomes
As you can see in the example above, risk scores are not just an abstract number; they are a direct representation of patient health. But the benefits of complete code capture go beyond RAF scores and compliance. Capturing patient health status at the highest level of specificity contributes to:
- Identification of additional care management needs
- Developing wellness/health incentive progress
- Disease intervention strategies
- Provider pre-visit planning
- Stabilization of beneficiary premium expense
All of these elements are critical to improving health outcomes at both the individual and population level—a win for for patients, plans, and providers alike.
 About the author
About the author
As chief operating officer of Episource, Erik Simonsen is responsible for the delivery of onshore and offshore coding services, record retrieval, IT infrastructure, and compliance. His knowledge in engineering, finance, and operations enables him to continuously improve performance and operational transparency for clients. He has over 10 years of experience managing outsourced centers, and substantive backgrounds in investment banking and technology. Erik has a BS in Biomedical Engineering from Johns Hopkins University and an MBA from NYU Stern.
