Rex Wallace, principal of Rex Wallace Consulting, takes a closer look at the Centers for Medicare & Medicaid Services’ announcement about data collection for Star ratings in the wake of COVID-19.

Earlier this week, the Centers for Medicare & Medicaid Services (CMS) notified Medicare Advantage (MA) plans of additional flexibility related to the 2019 Novel Coronavirus (COVID-19) and its impact on data collection for Star ratings.
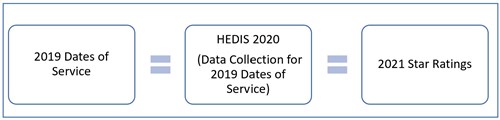
Most of the guidance addresses the upcoming 2021 Star ratings, due to be released this October. The 2021 Star ratings are based on 2019 performance, but a significant amount of the data for key categories is collected in 2020, either through the collection of medical records from provider offices (HEDIS ®) or through the administration of a patient/member experience survey (CAHPS) which is fielded to MA members.
RELATED: CMS announces changes to 2021- and 2022-Star ratings data calculations in response to COVID-19
The additional flexibility is provided in order to allow the health care system to respond to the COVID-19 pandemic, rather than focusing on data collection for Star ratings.
2021 Star ratings
HEDIS data collection
The newly released guidance eliminates the requirement for MA plans to submit HEDIS 2020 data (for 2019 dates of service), because of the burden placed on health care workers in the provider offices and the MA plans. Instead, CMS says it will use last year's HEDIS performance (measure-level rates and ratings, based on 2018 performance) for the 2021 Star ratings.
Normal:
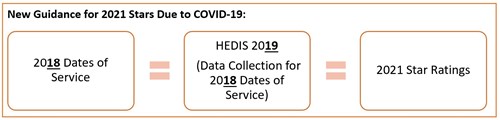
It is interesting that the wording does not say that plans cannot submit HEDIS 2020 data; it only says that CMS is removing the requirement to do so. In my discussions with many plans this week, the common belief is that CMS is definitely not planning to count HEDIS 2020 data. However, I would expect those plans that saw significant improvement in their 2019 dates of service to appeal to CMS in hopes of somehow using 2020 HEDIS rates, if only for the administrative HEDIS measures and not the hybrid measures.
CAHPS survey
The guidance also eliminates the requirement for MA plans to submit 2020 Consumer Assessment of Healthcare Providers & Systems survey data. CMS will use last year's CAHPS rates and ratings for the 2021 Star Ratings.
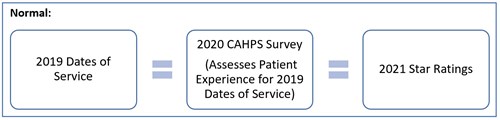
New guidance for 2021 Stars:

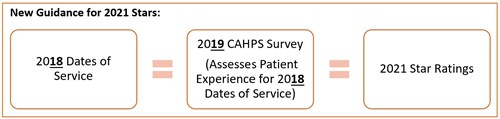
This is bad news for MA plans that made significant improvements in their member experience throughout 2019. It’s also important to note that the weights for eight of the nine CAHPS measures are slated to increase from 1.5 to 2 for 2021 Star ratings. There is no indication that this is no longer happening. Thus, plans that performed more poorly on 2019 CAHPS than they projected to perform on 2020 CAHPS (due to an improved patient/member experience) will not only fail to reap the benefits of that improved performance, but the low Star ratings from the 2019 CAHPS measures will be magnified due to their increasing weights for 2021 Stars.
Health Outcomes Survey (HOS)
The 2020 HOS survey is currently delayed from April until late summer, though CMS warns that further adjustments might be needed. It's not clear yet whether CMS might delay it further or possibly entirely forego a 2020 HOS survey and use last year's results for the 2022 and 2024 Star ratings.
All other measures
- The measurement period and data collection for all other measures will not change.
- If COVID-19 prevents CMS from being able to effectively validate this year’s Star ratings data, CMS will replace the data with last year's data.
- Should COVID-19 affect the ability to calculate 2021 Star ratings, CMS also reserves the right to simply re-apply the 2020 Star ratings as the 2021 Star ratings. Depending upon whether you improved or declined in performance in 2019, this could have a significant impact on your projected revenue in 2022.
- Newer contracts that would have had their first-ever rating for 2021 Star ratings will be considered "too new" for one additional year and will not receive a 2021 Star rating.
- For HEDIS and CAHPS measures that are part of the improvement measure calculation, CMS will use the improvement change from the 2020 Star ratings.
2022 Star ratings
As of now, CMS expects things to be measured normally next year, though they do expect performance to be lower as a result of COVID-19. Thus, they are delaying the implementation of the 5 percent cut point guardrails until January 1, 2021. This will allow cut points to decline more than 5 percent if needed to accurately reflect industry performance.
Regarding the improvement measures, CMS is expanding the “hold harmless rule” to include all contracts, since it expects performance to drop in 2020 compared to 2019 due to COVID-19. This means that contracts with 4+ Stars that would have had their overall rating decreased with the addition of the Improvement measures will be held harmless. Their Star rating would not be decreased from 4+.
Patients over paperwork
CMS also referenced the following in its published rule, related to members impacted by COVID-19:
- Flexibility to waive cost sharing and to provide expanded telehealth benefits:
- MA plans may waive cost-sharing for COVID-19 testing and expand telehealth services beyond what their 2020 benefits were designed to cover.
- Part D “refill-too-soon” edits and maximum day supply:
- Plans with Part D benefits may relax their “refill-too-soon” edits and allow enrollees to obtain the maximum extended day supply available under their plan, if requested and available.
- Home or mail delivery of Part D drugs:
- CMS is allowing plans with Part D benefits to relax plan-imposed policies that discourage home or mail delivery during this time.
- Audit Reviews:
- CMS is pausing activities that require them to ask providers for documentation, such as prior authorization reviews. CMS is also reprioritizing audit activities to allow focus on patient care.
Summary
In closing, we are grateful for this guidance from CMS during these turbulent times. It does not answer every question, but it is a good start. Although Star ratings are clearly not the most important thing happening in this industry right now, they are still critical for MA plans. One small result of the COVID-19 pandemic is that the quality improvement efforts of many MA plans over the past 12 months will likely yield no measurable results. A small consequence in the grand scheme, though still frustrating and disheartening. Know that you are not alone. If you focus on your members, your staff, and your invaluable health care partners, you will have done the best you could do.

 About the author
About the author
Rex Wallace is the principal of Rex Wallace Consulting, which aims to help Medicare Advantage plans perform at their highest levels and achieve higher Star ratings, resulting in improved outcomes, experiences, and quality of life for their members.
